Do you ever get that slimy feeling across your teeth? Maybe you haven’t brushed them well enough and you can feel a bit of a build up of a sticky substance clinging to your pearly whites? Well that slimy stuff is called Biofilm.
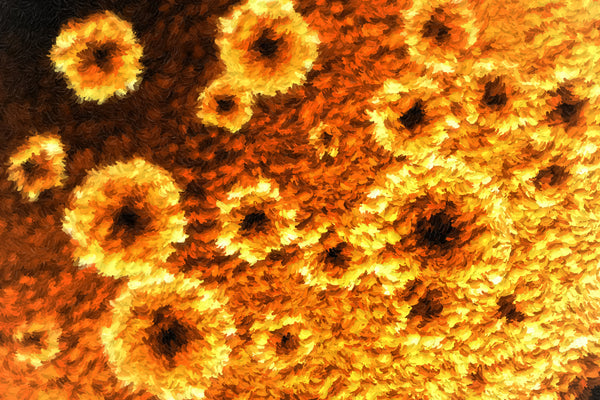
Biofilm is basically a sticky, glue-like substance that is produced by bacteria. Biofilm is an evolutionary safety-mechanism for bacteria, it is their way of not only sticking with their colony but also creating a safe environment for them to live in and flourish. Bacterial biofilms are prevalent on most wet surfaces including environmental, non-environmental and human bodily tissues and can contain different species of bacteria or just one specific type of bacteria. They can also harbour fungi, yeasts and other pathogenic microbes, which in turn, contribute to the production of the biofilm that is keeping them safe.
Now, before we get too involved about Biofilms, we need to know a little more about the bacteria that make them. For the use of microbiology and medicine bacteria are looked upon at either being planktonic (freely moving) or sessile (anchored). Generally, early medicine looked at bacterial infections as infections by planktonic bacteria. A pathogenic bacterium that has managed to fight its way through the body’s natural defence mechanisms and is floating around on its own, happy as can be making us sick. Antibiotics were developed on this concept. A bacterium invades our body, we take antibiotics, said bacteria dies and we’re healthy again. Simple right? No, not really…
You see planktonic bacteria can quite easily become sessile bacteria and sessile bacteria create biofilms. It’s just basic chemistry; a planktonic bacterium can adhere to any surface in an aqueous environment using a weak, reversible bond called van der waals forces. If the bacterium then likes what it sees, it creates a more permanent, irreversible bond and can join to other molecules via cellular adhesion. Basically this sees the proteins from one bacterial cell bind to the proteins of another bacterial cell to form a strong and permanent bond. Then cellular multiplication occurs as well as recruitment of other types of microbes. Small micro-colonies then form and they start enclosing themselves in a self produced polymeric-matrix, consisting of polysaccharides (a sticky/sugary substance) that form biofilms.
The strength and size of these biofilms are important for their multiplication as the larger they are and the more bacteria they contain makes them a more attractive adhesion site to passing bacteria and other microbes. This is how they ‘recruit’ and begin to engage in what is referred to as quorum sensing. This is essentially a means, of the bacteria within the biofilm, communicating with planktonic bacteria through the transmission of biochemical messages that encourage them to join and help colonize the biofilm. Planktonic bacteria are able to assess the density of the transmitting population and are more inclined to join if they sense that the colony is strong.
Why do bacteria create biofilms?
As I mentioned earlier, biofilms have formed as a part of bacterial evolution. It keeps them safe and also makes them stronger. Imagine this for a moment, you’re a soldier at war and you’re on your own, you come up and face the enemy, who do you think will win? Probably the enemy, especially if there is more of them and they are stronger. Now imagine you’re part of an army, not just any army an army that has soldiers with all different strengths and abilities. Some of the soldiers are really good at using a bow & arrow, some are really athletic and fit, some are excellent shooters, others have the ability to throw grenades with precision (lovely thought hey?!). Well if you were part of an army like this, how safe would you feel among your fellow soldiers, you’re army is bound to win most, if not all of the fights it is up against.
From an evolutionary standpoint, as anything evolves it gets stronger and learns to adapt and change to and with the surrounding environment. So bacteria and other microbes aren’t any different. For bacteria, the advantages of biofilm formation are numerous. These advantages include: protection from antibiotics and other anti-microbials, disinfectants and dynamic environments. Also, they are protected from our natural defences, our innate and adaptive immune responses – antibodies and our little own soldiers, specifically phagocytes (these are like little pac-men who float around engulfing all the bad guys). So not only are bacteria in biofilms strong and safe, one of the direct ways in which our immune system tries to destroy them also causes us ill health by creating immune-mediated chronic inflammation causing autoimmune and inflammatory conditions which I will describe in greater detail later.
Advantages of Bacteria in Biofilm
What is the impact of biofilms to our health?
Where do I start?!
Firstly, let’s just quickly re-hash that in terms of medical research, biofilms are a relatively new topic. This is mainly due to the fact that the popular belief was that the majority of bacteria lived planktonically and were easier to kill. So science believed that they kind of had bacterial infections covered. Obviously, until we started seeing the development of antibiotic resistant bacteria and more chronic bacterial infections, questions were raised and now with the emerging evidence of the great importance of our bacterial microbiome, there is even more focus driven into this area. Don’t get me wrong, microbiologists have known about biofilms for a very long time; however science has not connected them to human illness until the last couple of decades.
The way in which biofilms affect our health is extremely multifaceted, some are fairly simple, others much more complex, I’ll start by explaining some of the simple and go onto the more complex.
Obviously, biofilms can affect any surface or tissue in, on and around our body. From our teeth, to our skin, heart and of course gut.
Cystic Fibrosis (CF) sees the bacterium Pseudomonas aeruginosa as actually the leading cause of death. This bacterium gets a hold on the weakened lungs and can thrive due to the immunosuppressive nature of CF. It is hard to kill, obviously as it is in a strong biofilm and unfortunately, contributes to an increase in mucus coughed up by the CF patient and recurrent and chronic infections.
Legionnaire’s disease is a disease actually spread by biofilms. There is no human-to-human transmission of legionnaire’s diseases; the source of infection is Legionella pneumophila biofilms that are established in air conditioners, water fountains and hospital equipment that are resistant to disinfectants. Parts of the biofilm can break free, the bacteria can become planktonic, inhaled and they can then establish infection and biofilm in the human lungs.
Chronic otitis media (ear infections) in children is now being linked to bacterial biofilms in the middle ear. This is why antibiotics are no longer given (well they shouldn’t be) for ear infections and also why children who suffer from chronic otitis media actually respond very well to therapeutic grade Probiotic therapy and a general gut microbiome over hall as gut dysboisis is commonly a driving factor behind chronic otitis media- but that’s a story for another day!
Now for the gut, our favourite and this is where things may get more complex. If you imagine the research on biofilms as an arm, the involvement of biofilms in human health is the finger and the involvement of them in gut health is the finger nail, in-fact, possibly the tip of the finger nail. In terms of length of research, although it’s only the tip of the finger nail – we are at the start of what will turn out to be a very long rabbit hole and I believe the beginning of many, many more discoveries about the involvement of our gut microbiome in chronic health states.
Barrett’s Oesophagus (BO) arises when people suffer from chronic gastroesophageal reflux disease (GORD). A change to the cells lining the oesophagus actually happens and this can lead to oesophageal cancer. It has been shown that patients with BO have a high micro-colony rate of campylobacter species. What is interesting is that campylobacter is closely related to helicobacter species and helicobacter (H.pylori) biofilms are a known cause of stomach ulcers, stomach cancer and also reduced and/or increased stomach acid which leads to GORD and BO!
Inflammatory Bowel Disease (IBD) includes Ulcerative Colitis (UC) and Chrone’s Diseases (CD). There is now a widely held belief that gut bacteria are involved in the disease pathogenesis of IBD. Research into UC especially is suggesting that biofilm growth in the gut mucosal layer is involved in the pathogenesis as micro-colonies of bacteria are frequently seen in the gut lining of UC patients and UC also has a high resistance to anti-biotic therapy. Although antibiotic therapy seems to suppress UC symptomatically for a while, after the cessation of treatment the bacterial colonies and symptoms come back stronger suggesting their protection from the medications. Research into CD is also showing an increase of a specific type of E.coli that is more prevalent in CD sufferers and it is known that this type of E.coli has a greater biofilm-producing capacity.
Now, I mentioned earlier that one of the direct ways in which our natural defences try to protect us from pathogenic biofilms actually can start to harm us. This is because it can trigger autoimmune responses and inflammation. Remember above how I mentioned about phagocytes, they’re like a little pac-man running around eating the bad guys? Well if these guys are activated by our immune system and sent off to do a job but are unable to do it as the bacteria that triggered the signal in the first place are protected by a biofilm, they get ‘frustrated’, quite literally. In a process called frustrated phagocytosis phagocytes are activated but cannot engulf the bacteria in biofilms so they begin to secrete toxic compounds that damage nearby healthy host tissue. This, along with the larger production of antibodies is a possible causative factor for many autoimmune, inflammatory and oxidative stress conditions including IBD, autism, asthma, fibromyalgia, chronic fatigue syndrome and more, which can all also be linked back to initial gut dysboisis. In fact, research is now showing even lupus is now being linked back to this process. Remember that rabbit hole I mentioned?!
Can I get rid of Biofilm?
The short answer is yes.
The long answer is- the typical clinical scenario of a biofilm associated infection, is clinical resolution of the initial presenting symptoms while the patient is undergoing antibiotic therapy, i.e., the planktonic bacteria are cleared. However, shortly after antibiotic therapy is terminated the patient presents with symptoms identical to the initial presentation since bacteria in the biofilm state survived therapy and reinfected the host with planktonic cells. This is happening because the therapy is not breaking down the biofilm to target a majority of the sessile bacteria. Research is now suggesting that enzymatic therapy is beneficial as the enzymes actually break down the polymeric-matrix of the biofilm.
Combining this treatment with a diet rich in lacto-fermented bacteria to help establish a healthy, flourishing gut microbiome could possibly prevent, even subside many chronic conditions as we have seen here.
What can I do to prevent Biofilm Growth?
Lactoferrin is an abundant, iron-binding protein from the innate immune system. Found in greatest abundance in breast milk and cow milk, lactoferrin is generally thought of as a milk protein. However, lactoferrin is a multifunctional protein serving many roles. It was originally thought to just function as an iron transport protein in blood, but observation of lactoferrin in our white blood cells suggest that this protein might have a greater role in our innate immunity and it is found in abundance in the gut.
While anti-bacterial and anti-biofilm efficacy has been demonstrated for lactoferrin and its derivatives, the mechanism of action remains an area of active research. It is suggested that the iron-binding nature of lactoferrin may be the main mechanism of action in its anti-microbial and anti-biofilm process as iron, although it is an essential mineral for human survival, it is also an essential nutrient for bacteria and too much free iron provides the perfect, nutrient dense breeding environment for bacteria and the development of biofilms.
Here’s my absolute favourite part though, it just shows you how important our good bacteria are and just how intelligent our bodies are! Our lactic-acid bacteria, bifidobacterium and lactobacillus strains are resistant to lactoferrin’s anti-bacterial effects! Not only that, lactoferrin promotes the growth and reproduction of our bifido and lactobacillus strains and lactoferrin is found in abundance in a good, strong, healthy gut that is thriving with lactic acid bacteria! Wow! Go mother nature you wonderful thing!
So in a nut shell, consume lacto-fermented foods like our yoghurt and kefir, keep your lactic-acid bacteria thriving which will keep a healthy gut which will encourage the presence of lactoferrin to keep bad guys away all whilst promoting the growth of more good guys! The human body is really so amazing and if we treat it right it has its own healing powers! Just think if every time someone was sick health care would be focused on the gut? We would all live to 100 or more!
Summary
Biofilms are strong, powerful colonies of bacteria and pathogens that can affect our health in many different ways. Their presence is being linked to a plethora of chronic health conditions ranging from Inflammatory Bowel Disease to Lupus. Lactoferrin, an iron-binding protein and essential part of our innate immune system is vital in helping to keep the development of biofilms at bay. The presence of lactoferrin is also dependant on an abundance of our good, gut loving lactic-acid bacteria and vice-versa. So, in short- keep a healthy gut and a healthy gut will keep you! It really has such are large involvement in so many health conditions!
Interested to learn more?
Sign up to our FREE Online Parasite Workshop





