I’ve recently been perusing the medical databases looking at evidence and current research around constipation, and I must say… there is a LOT of research into constipation. Constipation in the disease state, constipation in children, constipation and Chinese herbs, constipation and pharmacological agents, systematic reviews, meta-analyses and so on! So much high level, extensive research…
And very little talk about repairing your digestive system, your microbiome and your diet.
If we’re going to talk poo (and it’s going to be fun), let’s get the boring bits out of the way.
Let’s Look At Some Definitions
- Motility – or gastric motility refers to the muscular contractions known as peristalsis that squeeze and push food along the gastrointestinal tract. This is important to know when we look at causes of constipation.
- Transit time – The time from ingestion of food to defecation.
- Microbiota – collection of microorganisms that exist with our gastrointestinal system. Their types and number can play a role in constipation.
- Constipation – difficult, incomplete, infrequent bowel motions may be painful with a sense of blockage.
- Functional constipation – also known as idiopathic constipation, meaning it does not have a known physical or physiological cause. There is no identifiable reason for this.
- Chronic constipation – symptoms of constipation lasting more than 3 months, including straining, hard stools, incomplete emptying, having to perform manual removal of stool, with less than 3 bowel movements per week. According to called the Rome IV criteria for functional gastrointestinal disorders, these symptoms must occur in more than 25% of bowel motions.
So…
Are You Constipated?
Poo is a big part of our social psyche, right? Poo jokes abound, poo songs, we obsess over our children’s poo, we’ve even written (a lot of) books about it, and we ALWAYS feel better after a good poo. Having a poo requires your parasympathetic nervous system to be in control and we get a little hit of happy hormones when we completely empty our bowel. There are whole aisles at the chemist dedicated to our bowels. Our toilets across the land are filled with books and magazines, which doesn’t tell us we love hanging out in there. It tells me things aren’t as free and easy as they should be when number twos come about.
Who’s At Risk For Constipation?
Well, everyone! The prevalence of constipation can be up to 29% in some areas. The general rates sit at an average of 14%; over the age of 60 the rate goes up to 30%. Interestingly, we see diversity and number of microbes in our gut drop as we age. Women are more prone than men, and the elderly in homes or institutions are also more highly affected. Those who eat a SAD – standard Australia diet high in processed foods will have higher rates of constipation. Children have higher risk of constipation. There are so many factors that either directly cause or at least play a role in constipation. I will list them here:
- Some medications – non steroidal anti-inflammatory medications, beta blockers, diuretics, and many more. Check your medication leaflet for listed side effects.
- Depression
- Immobility
- Some cancers (obstruction or affecting gut function)
- Thyroid imbalances
- Neuropathological diseases such as Parkinson's, multiple sclerosis or diabetic complications (neuropathy)
- Lifestyle factors – dehydration, sedentary lifestyle, low fibre (vegetables) diet
How Does Pooing Work?
Well, it’s simple yet complex! I’ll give you the simplified version. You have two sphincters, an internal and external sphincter – watch this ted talk with Guilia Enders who explains it with eloquence). The internal sphincter responds to stretch in the bowel wall, triggering the urge to use your bowels. This can be overridden by your external sphincter, which is under conscious control. We’ve all had times when we get the urge to poo but ignore it consciously – although this is not a great idea, but necessary at times. When the bowel fills with matter it stretches the bowel wall which triggers the release of serotonin. The serotonin triggers peristaltic waves throughout the bowel, leading to the movement of faeces towards the anal sphincter and triggering the urge to poo. This bowel motion can be dependent on a mix of conscious and subconscious triggers. It is affected by toilet training (habit), mood, preference, location, time of day. Who has ever heard someone say they cannot poo until they get home to their own toilet? A word of warning… sometimes choosing to hold it in can cause you to miss the boat, so to speak.
Serotonin isn’t the only neurotransmitter that influences peristalsis, however, melatonin also plays a role. In fact, melatonin levels in the gut can be up to 10 times higher than in the blood. Who would have thought that serotonin and melatonin play this role within our gastrointestinal system? The reason I am mentioning this is that these two hormones play a large and diverse role in our bodies. Their production is dependent on so many things that I always discuss your microbiome, movement, sunlight exposure, and so on. I would like you to understand that constipation involves so much more than extra fibre and extra fluids. Some of this will be explored below with a list of tips for improving your bowel motions in the long term.
What about laxatives? A lot of laxatives will create (sometimes painful) peristaltic contractions within the bowel but do nothing to address the underlying issues. One large-scale review of constipation in childhood concluded the use of laxatives were safe but listed commonly occurring side effects such as flatulence, abdominal pain, nausea, diarrhoea and headache. Is this really what we are after? Pharmacologically assisted bowel motions with a side effect profile that affects your daily life?
Improving Your Visits To The Throne Room
Stretch – this is a very basic recommendation. Increase your vegetable consumption. It has the necessary fibre to not only bulk out and create stretch in the bowel wall but to feed your microbiome and help create a healthy colon.
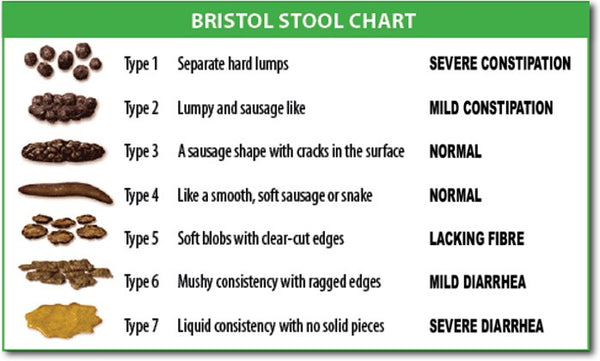
Probiotics – the bulk of people with chronic constipation have low numbers of beneficial bacteria in their gut. Research has shown that probiotics may improve how long it takes to move food through the bowel (transit time), and the frequency and consistency of stool. Functional food-based probiotics such as our coconut water kefir and coconut yoghurt can add to the formation and passing of a nice number 4 on the Bristol stool chart.
Deal with your gut infections – when the gut is overridden by infection, whether they be bacterial, fungal, parasites or a combination, you are going to have dysfunctional bowel function. Did you know pathogenic flora can paralyse the bowel wall? They can paralyse the oesophageal sphincter contributing to reflux and they can inhibit peristalsis contributing to constipation. Gut infections have an immense impact on many aspects of everyday health and wellbeing. Managing gut health is a specialty of Kultured Wellness and there are guided programs, consultations and one-on-one programs available here.
Hydration – this is as basic as fibre. How much water are you drinking really? If you are dehydrated, there will be no fluid reserved for bulking out your stools and allowing a bowel motion that is moist and properly formed. It will be hard, dry and difficult to pass – leading to chronic constipation with a very simple solution.
Hormones – once again, correcting your gut, moving your body, eating whole foods , good fats, a vegetable-dense diet, sleeping, and getting sun exposure. I say it so many times, this ancestral, natural, aligned and balanced way of living and interacting with our gorgeous planet will help balance and align us, our hormones, and our bowels. Serotonin and melatonin will be so much better balanced when all of your body systems, including the gut microbiome, are functioning optimally. These lifestyle interventions have a very real effect on your constipation.
Targeted probiotic interventions – we are just at the very beginning of research into the microbiome and probiotic treatments, but it is exciting times. Some of the emerging evidence about the highly studied E. coli Nissile 1917 (in the form of Mutaflor) can assist with constipation.
Targeted foods for constipation – high mucilage foods such as flax and chia attract large amounts of fluid and can bulk out the bowel, help restore the mucous layer in the gut and ease the path forward. Whole flax at night mixed in a glass of water can help some people with their constipation. Vegetables, vegetables, vegetables!
Short-term interventions while addressing the underlying cause – I am a big fan of enemas. You can read my article on enemas here. There are numerous benefits for our bodies besides managing constipation. Enemas are a very gentle, less offensive way to remove impacted stool from the bowel and it does not cause rebound constipation or affect your ability to pass a normal stool. They will keep you on top of your toxic load while you dig deeper into the causes.
What Does A Good Poo Look Like Anyway?
- Well, it comes every day, once or twice
- It is formed
- It does not have any particularly offensive and abnormal smell
- It is medium brown in colour
- It is passed with relative ease – you should not sit on the throne long enough to read that magazine
- It is a number four on the Bristol stool chart
So now you know what a good poo looks like, some of the risk factors for constipation and some of the interventions that may help. There are so many more factors and complexities beyond the scope of this article; however, there are some things you can do right now to get things moving along...
In A Nutshell
- Keep your fluids up (don’t just read this – go and get a drink now… go on!)
- Keep your intake of plant fibres high. Aim for 6-9 cups of vegetables per day
- Move your body
- Manage gut infections
- Consume probiotic foods daily
- Balance and align your body's natural function including hormonal function with the correct diet and lifestyle
- Consider targeted interventions such as probiotic supplements and enemas, if needed
Resources
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5774595/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5673021/
- https://www.ncbi.nlm.nih.gov/pubmed/25099542
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5446139/
- https://www.mdedge.com/ccjm/article/136631/drug-therapy/chronic-constipation-update-management




